Our Group organises 3000+ Global Events every year across USA, Europe & Asia with support from 1000 more scientific Societies and Publishes 700+ Open 91��ɫ Journals which contains over 50000 eminent personalities, reputed scientists as editorial board members.
Open 91��ɫ Journals gaining more Readers and Citations
700 Journals and 15,000,000 Readers Each Journal is getting 25,000+ Readers
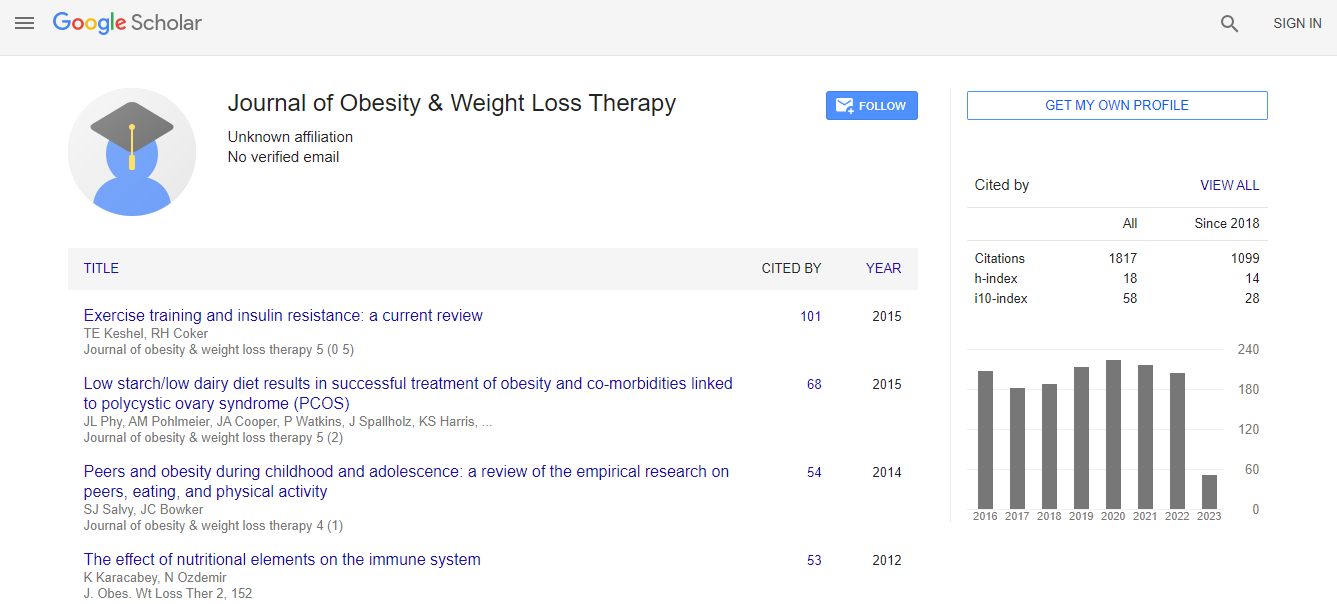
Citations : 2305
Indexed In
- Index Copernicus
- Google Scholar
- Open J Gate
- Genamics JournalSeek
- Centre for Agriculture and Biosciences International (CABI)
- RefSeek
- Hamdard University
- EBSCO A-Z
- OCLC- WorldCat
- SWB online catalog
- CABI full text
- Cab direct
- Publons
- Geneva Foundation for Medical Education and Research
- Euro Pub
- University of Bristol
- Pubmed
- ICMJE
Useful Links
Recommended Journals
Related Subjects
Share This Page
Changes in liver metabolism in Mg2+ deficiency: Implications for NAFLD and metabolic syndrome
3rd International Conference and Exhibition on Obesity & Weight Management
Andrea M P Romani, Chesinta Voma, Lauren Keenan, Coleen Croniger and Michelle Puckowic
Case Western Reserve University, USA
ScientificTracks Abstracts-Workshop: J Obes Weight Loss Ther
DOI:
Abstract
Metabolic Syndrome, a pathological condition affecting approximately one-third of the USA population, is characterized by obesity, hepatic steatosis, insulin resistance, and hypertension among other medical conditions, and represents the single most common condition predisposing to diabetes and hypertension. Within this contest, liver steatosis is considered the hepatic representation of the disease and is currently classified as NAFLD. Hypomagnesaemia has been consistently observed in association with metabolic syndrome, and recent data from our laboratory suggest low Mg2+ level in the circulation and within the hepatocytes promotes dysmetabolic conditions typical of the metabolic syndrome. Rats exposed for 2 weeks to a 40% Mg2+ deficient diet present a 2-3 fold increase in intrahepatic triglyceride content associated with a marked increase in numerous genes involved in fatty acid synthesis including IRS2, SREBP1c, PPAR�?³, FAS, LCAD, HMG-CoA reductase and HMG-CoA synthethase. PPAR-�?±, instead remained unaltered. The upregulation of IRS2 contrasted the downregulation of IRS- 1 and pAkt, leading to decreased glucose accumulation, and attenuated insulin signaling. As a result of this altered signaling Fox-01 remained active and resulted in the upregulation of the gluconeogenic genes PEPCK and F, 16 BPase. Additionally, the reticular hexose 6-phosphate dehydrogenase (H6PD) and the coupled 11�?²-hydroxysteroid dehydrogenase-1 (11-�?²-HSD1) were both 3-4 fold upregulated in gene and protein expression, resulting in the significant production of intraluminal NADPH and cortisol levels. Taken together, our results provide compelling evidence that reduced extracellular Mg2+ level precedes and promotes metabolic syndrome onset in that: 1) liver metabolism undergoes a switch from glucose-based to fatty acidbased synthesis with minimal changes in catabolism, resulting in the increased deposition of intrahepatic triglycerides; 2) increased cortisol production, and 3) reduced insulin responsiveness. The majority of these gene dysregulation trended towards renormalization following the restoration of normal extracellular and cellular Mg2+ content.Biography
Andrea M P Romani, MD, PhD obtained his medical degree from the University of Siena, Italy and his PhD from the University of Turin, Italy. He completed his postdoctoral studies under Dr. Scarpa, in the Department of Physiology and Biophysics, Case Western Reserve University, Cleveland, OH. He is currently Associate Professor in the Department of Physiology and Biophysics at Case Western Reserve University, Cleveland, OH. He has published almost 90 peer review articles in high profile journals together with numerous invited reviews and book chapters. He is currently serving as an Editorial Board Member for Archives of Biochemistry and Biophysics, Magnesium Research, World Journal of Gastro-Intestinal Physio-Pathology among others.
Email: amr5@case.edu