Our Group organises 3000+ Global Events every year across USA, Europe & Asia with support from 1000 more scientific Societies and Publishes 700+ Open 91��ɫ Journals which contains over 50000 eminent personalities, reputed scientists as editorial board members.
Open 91��ɫ Journals gaining more Readers and Citations
700 Journals and 15,000,000 Readers Each Journal is getting 25,000+ Readers
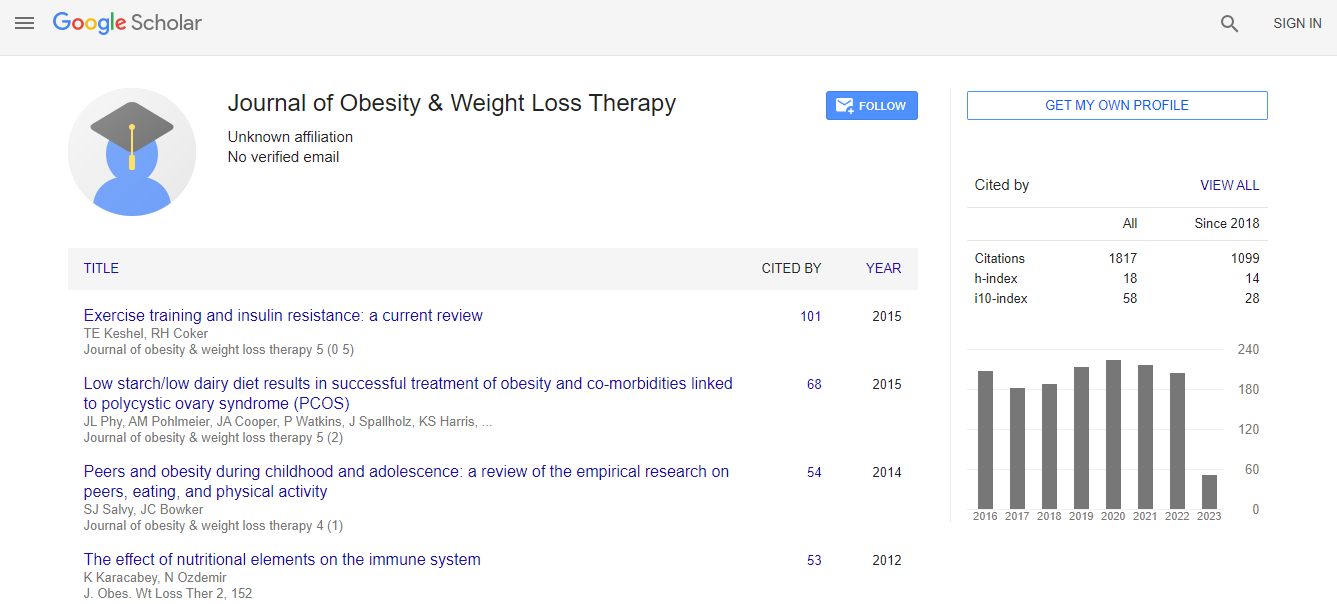
Citations : 2305
Indexed In
- Index Copernicus
- Google Scholar
- Open J Gate
- Genamics JournalSeek
- Centre for Agriculture and Biosciences International (CABI)
- RefSeek
- Hamdard University
- EBSCO A-Z
- OCLC- WorldCat
- SWB online catalog
- CABI full text
- Cab direct
- Publons
- Geneva Foundation for Medical Education and Research
- Euro Pub
- University of Bristol
- Pubmed
- ICMJE
Useful Links
Recommended Journals
Related Subjects
Share This Page
Metformin inhibits glucose production in hepatocytes by activating AMPK
3rd International Conference and Exhibition on Obesity & Weight Management
Ling He
Johns Hopkins University School of Medicine, USA
ScientificTracks Abstracts-Workshop: J Obes Weight Loss Ther
DOI:
Abstract
Metformin is a first-line anti-diabetic agent taken by 150 million people across the world every year. Metformin has been shown to reduce BMI and improve hyperglycemia and insulin resistance in obese and diabetic patients. Due to these benefits, there has been an increase in its use by obese children. However, its mechanism of action remains only partially understood and controversial. It has been proposed that metformin suppression of glucose production via the inhibition of mitochondrial respiratory chain complex 1 increases the AMP/ATP ratio in hepatocytes and is AMPK-independent. However, unachievably high concentrations of metformin were employed in these studies. We found that metformin, via an AMPK-dependent mechanism, suppresses glucose production and gluconeogenic gene expression in primary hepatocytes at concentrations found in the portal vein of animals (60-80 �?¼M) without increasing the AMP/ATP ratio. Interestingly, low concentrations of metformin actually increased cellular ATP levels. Metformin also inhibits gluconeogenic gene expression in the liver of mice when administered orally. Low concentrations of metformin promote the formation of the AMPK �?±�?²�?³ complex, which leads to increased phosphorylation of AMPK�?± at T172 by LKB1 and reduced dephosphorylation of AMPK�?± at T172 by protein phosphatase PP2C in in vitro assays, resulting in an increase in net phosphorylation of the �?± catalytic subunit at T172. Furthermore, the cAMP-PKA pathway negatively regulates AMPK activity through phosphorylation at S485/497 on the �?± subunit, which in turn reduces net phosphorylation at T172. Since diabetic patients often have hyperglucagonemia, AMPK�?± phosphorylation at S485/497 is a therapeutic target to improve metformin efficacy.Biography
Ling He graduated from University of Arkansas for Medical Sciences, USA. He did his postdoctoral training in Dr. Fredric Wondisford’s laboratory at Johns Hopkins Hospital and Johns Hopkins School of Medicine, USA. Then he was recruited as an instructor and now is an assistant professor at the Divisions of Endocrinology and Metabolism, Department of Pediatrics at Johns Hopkins Hospital. His research focuses on the mechanistic study to understand the gene regulation of hepatic gluconeogenesis and lipogenesis.
Email: heling@jhmi.edu